Table of Contents >> Show >> Hide
- What Is Hyperlordosis?
- Common Symptoms of Hyperlordosis
- Main Causes and Risk Factors
- How Hyperlordosis Is Diagnosed
- Treatment Options for Hyperlordosis
- Best Exercises for Hyperlordosis (With Caution)
- Prevention and Everyday Posture Tips
- When to See a Doctor Right Away
- Real-Life Experiences: Living With and Treating Hyperlordosis
- Article Summary and SEO Details
If you’ve ever caught a side view of yourself in a mirror and thought,
“Whoa, why is my lower back doing that dramatic curve?” you might have
wondered about hyperlordosis. Often nicknamed “swayback,” this condition
happens when the normal inward curve of your lower spine becomes
exaggerated, sometimes causing pain, stiffness, and very unhappy back
muscles.
The good news: hyperlordosis is often manageable with the right mix of
stretching, strengthening, and lifestyle changes. In many cases, it doesn’t
require surgery or extreme interventions. Understanding what’s going on
in your spine is the first step to feeling better and standing taller.
What Is Hyperlordosis?
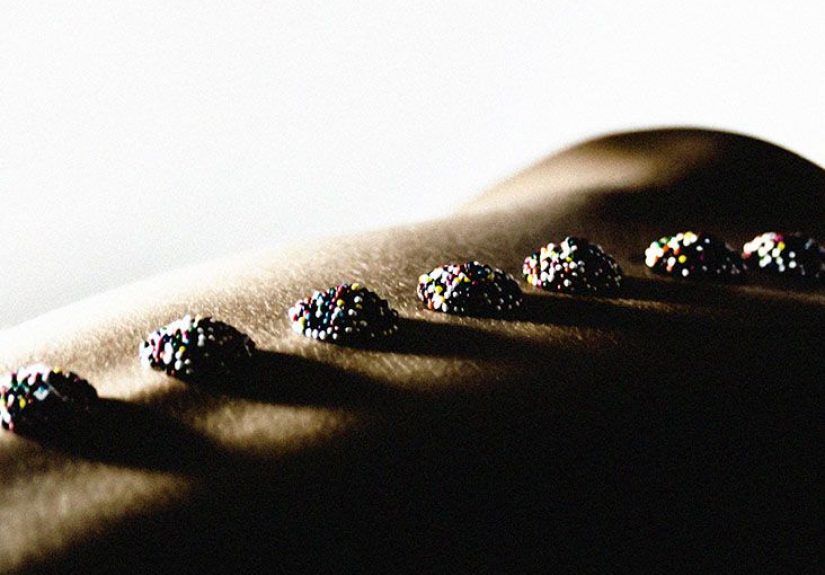
Your spine isn’t meant to be perfectly straight. From the side, a healthy
spine has gentle curves: a small inward curve in the neck and lower back
(lordosis) and a slight outward curve in the upper back (kyphosis).
Hyperlordosis refers to an excessive inward curve, most
commonly in the lumbar (lower) spine.
People with hyperlordosis often look like their pelvis is tipped forward,
their stomach and chest are pushed out, and their buttocks are more
pronounced. This posture can put extra stress on the vertebrae, discs, and
surrounding muscles, sometimes leading to lower back pain, muscle
tightness, or fatigue, especially after standing or sitting for long
periods.
Common Symptoms of Hyperlordosis
Hyperlordosis can look a little different from person to person. Some
people mainly notice the appearance of their posture; others feel more
pain than they see. Typical symptoms may include:
- A visible exaggerated inward curve in the lower back
-
Pelvis tilting forward, with the buttocks sticking out and the abdomen
protruding -
Lower back pain or discomfort, especially after long periods of standing,
walking, or sitting - Tightness in the lower back, hip flexors, or hamstrings
- Core and glute muscles that feel weak or “switched off”
- Reduced flexibility in the hips or lower back
-
In more serious cases, radiating pain, tingling, or weakness in the legs
if nerves are irritated
Mild cases may cause little to no pain and are found only during a routine
physical exam. More pronounced curvature or symptoms that affect walking,
sleep, or daily function deserve prompt medical attention.
Main Causes and Risk Factors
Hyperlordosis doesn’t usually appear out of nowhere. Often, it’s the
result of a combination of posture habits, muscle imbalances, and, in some
cases, underlying spinal conditions. Common causes and risk factors
include:
1. Poor posture and sedentary lifestyle
Long hours of sitting, especially slouched at a desk or hunched over a
phone, can weaken the core and glute muscles while tightening the hip
flexors and lower back. Over time, this imbalance can pull the pelvis into
an anterior tilt, exaggerating the lumbar curve.
2. Weak core and glute muscles
Think of your core and glutes as the natural “corset” and “support beams”
for your spine. When they’re weak, your lower back muscles often work
overtime to hold you upright, which can deepen the lumbar curve and lead
to soreness.
3. Excess body weight or pregnancy
Extra weight in the abdominal area – from obesity or pregnancy – shifts
the body’s center of gravity forward. To compensate, the lower back may
arch more to keep you balanced. For many pregnant people, this change is
temporary; for others, poor post-pregnancy posture can make it linger.
4. Footwear and movement habits
Frequently wearing high heels can push the hips forward and accentuate
lumbar lordosis. Certain sports or activities that emphasize back
extension (like gymnastics, dance, or some strength training styles) may
also contribute if not balanced with proper core and hip work.
5. Underlying spinal conditions
Sometimes, hyperlordosis is a side effect of other structural problems,
such as spondylolisthesis (slippage of one vertebra over another),
congenital spine differences, prior spinal surgery, or conditions like
kyphosis in the upper back. In these cases, treating the root cause is
just as important as working on posture.
How Hyperlordosis Is Diagnosed
Only a healthcare professional can diagnose hyperlordosis and determine
whether it’s simply a posture issue or part of a more complex spinal
problem. Here’s how the process usually works.
1. Medical history and physical exam
Your provider will ask about your symptoms, daily activities, work setup,
exercise habits, and any prior injuries or surgeries. During the physical
exam, they will:
- Observe your posture while standing, walking, and sometimes sitting
-
Look at your spine from the side to see whether the lower back curve
looks exaggerated -
Check whether the curve is flexible – for instance, does it decrease
when you bend forward or tuck your pelvis? -
Test muscle strength, flexibility, and sometimes reflexes and sensation
in the legs
2. The simple “wall test”
Providers sometimes describe a quick at-home posture check, often called
the “wall test”:
- Stand with your back against a wall, heels about 2 inches away.
- Keep your head, shoulder blades, and buttocks touching the wall.
- Slip one hand behind the small of your back at the level of your waist.
A small space is normal, but if you can fit more than one hand or there is
a large gap between your back and the wall, it may suggest an excessive
lumbar curve. This test isn’t a diagnosis by itself, but it can be a
helpful clue to bring up with your provider.
3. Imaging tests
If the curve looks significant, or if you have red-flag symptoms like
weakness, numbness, or bowel/bladder changes, your provider may order
imaging:
-
X-rays to measure the exact angle of the curvature and
check bone alignment -
MRI if there’s concern about discs, nerves, or other
soft tissues -
CT scans in certain complex cases to give more detailed
bone images
These tests help distinguish simple postural hyperlordosis from structural
conditions that might need more targeted treatment.
Treatment Options for Hyperlordosis
Treatment is highly individualized and depends on whether the curve is
flexible, how severe it is, and what’s causing it. The big picture is
usually the same, though: reduce pain, restore better alignment, and
protect your spine over the long term.
1. Lifestyle changes and home care
-
Posture awareness: Noticing when you’re over-arching
your back is step one. Many people benefit from gentle reminders – phone
alarms, sticky notes, or posture apps – to “reset” their alignment
throughout the day. -
Ergonomics: Adjust your chair, screen height, and
keyboard so you can sit with your feet flat, hips and knees at about
90° angles, and your ears roughly over your shoulders instead of in
front of them. -
Footwear: Limiting high heels and choosing supportive
shoes can help reduce forward pelvic tilt and strain on the lower back. -
Weight management: For some people, losing excess
weight around the midsection can reduce the “pull” that exaggerates the
lumbar curve.
2. Physical therapy and targeted exercise
For many people, physical therapy is the cornerstone of treatment. A
physical therapist can:
- Identify which muscles are weak and which are tight
-
Build a customized plan to strengthen the core, glutes, and hips while
gently stretching the lower back and hip flexors - Teach you how to find and maintain a neutral spine during daily tasks
- Progress your program safely as your strength and mobility improve
3. Medications and short-term pain relief
For flare-ups, your provider may suggest:
-
Over-the-counter pain relievers or anti-inflammatory medications, if
they’re safe for you - Occasional use of heat or cold packs
-
Short-term muscle relaxants in certain cases, if prescribed, to calm
muscle spasm
These tools can make it easier to participate in exercise and physical
therapy, but they don’t correct the curvature by themselves.
4. Bracing or surgery (in select cases)
Most adults with postural hyperlordosis never need surgery. Bracing is
sometimes used in children or teens with structural spine curves. Surgery
is usually reserved for cases where:
-
There is a significant structural deformity causing nerve compression or
progressive disability -
Underlying conditions like severe spondylolisthesis or other spinal
disorders are present -
Conservative treatments have failed and symptoms significantly affect
quality of life
If surgery is ever on the table, your spine specialist will walk you
through the goals, risks, and recovery process in detail.
Best Exercises for Hyperlordosis (With Caution)
Before trying any new exercise routine, especially if you have back pain,
it’s important to talk with a healthcare provider or physical therapist.
Stop immediately and seek medical advice if an exercise causes sharp,
worsening, or radiating pain.
1. Neutral spine practice at the wall
Stand against a wall as in the wall test. Gently tighten your abdominal
muscles and think of drawing your ribs down toward your pelvis, without
tucking your tail under dramatically. You’re aiming to reduce the gap
behind your lower back until it feels “just right” – enough space for one
hand, not a stack of books. Hold for 10–15 seconds, breathe, and repeat.
2. Pelvic tilts
Lie on your back with your knees bent and feet flat. Inhale, then exhale
as you gently tilt your pelvis so your lower back presses lightly into the
floor. Imagine zipping up a tight pair of jeans. Hold for a few seconds,
then relax. Repeat 10–15 times. This builds awareness of how to move your
pelvis out of an exaggerated arch.
3. Knee-to-chest stretch
Lying on your back, gently bring one knee toward your chest until you feel
a comfortable stretch in the lower back and glute. Hold for 20–30 seconds
and switch sides. You can also bring both knees toward your chest if it
feels good and doesn’t cause pain.
4. Child’s pose or kneeling back stretch
From a kneeling position, sit back toward your heels and reach your arms
forward on the floor, allowing your spine to gently lengthen. Breathe
deeply and hold the stretch for 20–30 seconds. This can help relieve
tightness in the lower back after a long day.
5. Planks and “dead bug” exercises
Core strengthening doesn’t have to mean endless sit-ups. Try:
-
Forearm plank: Maintain a straight line from head to
heels while gently bracing your core, avoiding letting your lower back
sag. -
Dead bug: Lie on your back with your hips and knees at
90°. Brace your core, then slowly lower opposite arm and leg toward the
floor without arching your back. Return and switch sides.
6. Hip flexor stretch
Kneel on one knee with the other foot in front, forming a 90° angle at
both knees. Gently shift your weight forward, keeping your torso tall,
until you feel a stretch in the front of your hip on the kneeling side.
Tight hip flexors are common in people who sit a lot and can contribute to
that excessive curve.
7. Glute bridges
Lying on your back with knees bent, press your feet into the floor,
squeeze your glutes, and lift your hips until your body forms a line from
shoulders to knees. Avoid over-arching your lower back at the top – the
power should come from your glutes, not from jamming your spine into
extension. Lower slowly and repeat 10–15 times.
Prevention and Everyday Posture Tips
Even after your symptoms improve, keeping your spine happy is an ongoing
project. Small, consistent habits often beat dramatic once-in-a-while
efforts. Helpful strategies include:
- Taking movement breaks every 30–60 minutes if you sit or stand a lot
-
Mixing strength training with flexibility work, not just focusing on
one -
Practicing body awareness – noticing when you’re arching your back and
gently resetting to neutral -
Using pillows or lumbar supports thoughtfully when sitting or sleeping,
rather than locking your back into an exaggerated position - Warming up before workouts that involve heavy lifting or jumping
When to See a Doctor Right Away
While many cases of hyperlordosis are mild and improve with exercise and
posture changes, some symptoms should never be ignored. Seek urgent
medical care if you have:
- Sudden, severe back pain after a fall, accident, or injury
- Back pain with fever, chills, or unexplained weight loss
- Numbness, tingling, or weakness in one or both legs
- Trouble walking, frequent tripping, or feeling that your legs “give out”
-
Difficulty controlling your bladder or bowels – this is a medical
emergency
These could signal a more serious spine or nerve problem that needs prompt
evaluation.
Real-Life Experiences: Living With and Treating Hyperlordosis
Reading about hyperlordosis in clinical language is helpful, but what
often matters most is how it plays out in everyday life. While everyone’s
story is unique, certain experiences come up again and again when people
talk about managing swayback posture.
“The Office Worker Curve”
Imagine a 32-year-old office worker who spends most of the day at a
laptop. Their lower back aches by late afternoon, and photos from the side
show a pronounced arch. At first, they assume they just “have a bad back”
and occasionally pop a pain reliever. Over time, that quick fix stops
working.
After finally seeing a provider, they’re referred to physical therapy.
There, they learn that the issue isn’t just their spine – it’s everything
around it. Tight hip flexors from sitting, weak glutes from not using them
much, and a habit of standing with their hips pushed forward all
contribute to hyperlordosis. Once they start doing daily core work, hip
stretches, and adjust their desk setup, their pain doesn’t vanish
overnight, but three months later they notice they can get through the
workday with far less discomfort.
The Teen Athlete
Another common story involves a teen athlete – maybe a gymnast, dancer, or
cheerleader – praised for a dramatic “arched” back. What looks impressive
for certain skills can, over time, strain the lower spine if it’s not
balanced with good core and hip strength.
A sports medicine clinician or physical therapist might explain that the
goal is not to flatten the back completely but to teach the athlete how to
move in and out of extension safely. They work on planks, bridges, and
controlled spine movements, as well as technique changes. The teen often
reports that not only does their back feel better, their overall
performance improves because they feel more stable in jumps, landings, and
turns.
The New Parent
New parents often develop hyperlordosis habits without realizing it. Think
about all the time spent carrying a baby on one hip, bending over cribs,
and leaning forward at changing tables. Add fatigue and lack of exercise,
and it’s no surprise the lower back starts complaining.
When a new parent finally has a chance to address their pain, they might
learn simple changes that make a big difference: alternating sides when
holding the baby, bending at the hips and knees instead of folding from
the waist, and doing short home exercise sessions during nap time. They
may not have an hour for the gym, but 10–15 minutes of targeted exercises
a few days a week can help retrain posture and ease strain.
What People Say Actually Helps
Across many of these lived experiences, a few themes repeat:
-
Consistency beats intensity. People often notice the
biggest improvements when they commit to small, regular changes rather
than rare, intense “fixes.” -
Awareness is powerful. Learning what neutral spine
feels like – instead of extremes of “slouch” and “military posture” –
helps people adjust throughout the day without obsessing. -
Support matters. Having guidance from a physical
therapist, trainer, or clinician reduces guesswork and fear. It’s
reassuring to know which movements are safe and which to modify. -
Progress is rarely linear. Many people describe good
weeks and bad weeks. Knowing that setbacks are normal makes it easier to
stay with the plan instead of giving up at the first flare.
While stories differ, one common thread is this: understanding hyperlordosis,
taking it seriously (but not fearfully), and working with professionals
when needed helps people move from “My back is just broken” to “I know
what’s going on, and I have tools to manage it.”
Article Summary and SEO Details
Hyperlordosis, or swayback, is an exaggerated inward curve of the lower
spine that can cause pain, stiffness, and posture changes. For many
people, it’s driven by a mix of modern lifestyle habits – prolonged
sitting, weak core and glute muscles, and tight hip flexors – sometimes
combined with underlying spinal conditions. Diagnosis involves a careful
physical exam and, when necessary, imaging studies. Treatment usually
focuses on physical therapy, posture correction, and lifestyle changes,
with medications or more invasive options reserved for select cases.
The big takeaway: hyperlordosis is often manageable. With guidance from a
healthcare professional, targeted exercises, and consistent everyday
habits, many people can reduce pain, improve posture, and protect their
spine for the long term.
SEO details






