Table of Contents >> Show >> Hide
- What is atherosclerosis (and how is it different from arteriosclerosis)?
- How plaque builds up inside arteries
- Where atherosclerosis can occur in the body
- Causes and major risk factors
- Symptoms of atherosclerosis: often silent, sometimes dramatic
- Potential complications
- How atherosclerosis is diagnosed
- Treatment: slowing, stabilizing, and sometimes opening arteries
- Prevention and everyday heart-healthy habits
- Real-life experiences and practical lessons
- When to talk to a healthcare professional
- Bottom line
If arteries were highways, atherosclerosis would be the slow-motion traffic jam you don’t notice
until everything suddenly stops. Plaque quietly builds up along the inner walls, the passage for
blood gets tighter, and one day that “mild narrowing” turns into a heart attack, stroke, or
painful legs after a short walk. Not exactly the kind of surprise anyone wants.
The good news? Atherosclerosis is common, but it’s also highly influenced by daily
choiceswhat you eat, whether you move, if you smoke, how you manage stress and chronic
conditions. Understanding what’s happening inside those blood vessels can help you protect your
heart, brain, and the rest of your body for the long run.
What is atherosclerosis (and how is it different from arteriosclerosis)?
The words are long, the difference is simple:
-
Arteriosclerosis is the general term for “hardening of the arteries.” As we age,
artery walls can become thicker, stiffer, and less flexible. Think of an old garden hose that
doesn’t bend as easily. -
Atherosclerosis is a specific type of arteriosclerosis in which
plaquemade of cholesterol, fats, calcium, and other substancesbuilds up inside the
artery walls and narrows the space where blood flows.
You can think of arteriosclerosis as the big category and atherosclerosis as one of the main
troublemakers inside that category. Atherosclerosis is especially important because plaque can
suddenly rupture, triggering blood clots that block arteries and cause heart attacks, strokes, or
other emergencies.
How plaque builds up inside arteries
Atherosclerosis doesn’t appear overnight. It usually starts early in life and slowly progresses
over years or decades. Here’s the basic storyline inside an artery:
1. Endothelial damage
Arteries are lined with a thin, delicate layer of cells called the endothelium. High blood
pressure, smoking, high LDL (“bad”) cholesterol, high blood sugar, and chronic inflammation can
irritate and damage this lining. Little microscopic “injuries” make the inner wall stickier.
2. LDL sneaks in and gets trapped
Once the inner wall is damaged, LDL cholesterol particles can slip beneath the surface and get
stuck. There, they can become oxidizedbasically “rancid” cholesterol. The immune system notices
something’s off and sends in white blood cells to clean up the mess.
3. Foam cells and fatty streaks
The white blood cells gobble up oxidized LDL and turn into “foam cells.” Clusters of foam cells
create a fatty streak along the artery wall. At this stage, atherosclerosis is already in motion,
but you won’t feel a thing.
4. Growing plaque and narrowing arteries
Over time, more fat, cholesterol, inflammatory cells, and scar tissue accumulate. A fibrous cap
forms over this mixture, and the whole structure bulges into the artery. The artery narrows, so
less blood can flow through, especially during times of higher demand, like exercise or stress.
5. Plaque rupture and clots
The most dangerous moment is when the fibrous cap cracks or ruptures. The body reacts by forming a
blood clot. If the clot blocks the artery completely, it can cause a heart attack, stroke, or
other sudden, life-threatening event. This is why atherosclerosis can be silent for years and then
suddenly become an emergency.
Where atherosclerosis can occur in the body
Atherosclerosis can affect almost any medium or large artery, so the symptoms depend on
where the narrowing happens:
-
Coronary arteries (heart): When plaque builds up here, it’s called
coronary artery disease (CAD). Reduced blood flow to the heart muscle can cause chest
pain (angina) or heart attacks. -
Carotid and brain arteries: Narrowing in the arteries supplying the brain can
cause carotid artery disease, transient ischemic attacks (“mini-strokes”), or major strokes. -
Peripheral arteries (legs and arms): This is called
peripheral artery disease (PAD). Reduced blood flow to the legs can cause pain when
walking and slow wound healing. -
Renal arteries (kidneys): Plaque in these arteries can contribute to high blood
pressure and kidney damage. -
Aorta: Atherosclerosis can weaken the wall of the body’s main artery, increasing
the risk of aneurysms (dangerous ballooning of the vessel).
Causes and major risk factors
There isn’t one single cause of atherosclerosis. It’s more like a team effort from genes,
lifestyle, and other health conditions. Risk factors fall into two big groups: things you
can’t change and things you can.
Non-modifiable (you can’t control these)
- Age: The older you get, the more time plaque has had to build up.
-
Sex: Men tend to develop symptomatic atherosclerosis earlier, but women’s risk
jumps after menopause. -
Family history: If close relatives developed heart disease or stroke at a young
age, your risk is higher. -
Genetic conditions: Disorders like familial hypercholesterolemia can cause very
high LDL cholesterol from a young age.
Modifiable (you have real power here)
-
High LDL cholesterol and triglycerides: Excess circulating fats contribute
directly to plaque buildup. -
Low HDL (“good”) cholesterol: HDL helps carry cholesterol away from arteries to
the liver for removal. Lower HDL means less cleanup. -
High blood pressure: Constant high pressure damages the artery lining, making it
easier for plaque to form. -
Smoking and vaping nicotine: Tobacco and nicotine products injure the
endothelium, lower HDL, and accelerate plaque formation. -
Diabetes and prediabetes: High blood sugar damages arteries and often comes
along with abnormal cholesterol and high blood pressure. -
Obesity and excess belly fat: Extra weight is linked with high blood pressure,
abnormal cholesterol, and insulin resistance. -
Lack of physical activity: Being sedentary reduces HDL, promotes weight gain,
and worsens many other risk factors. -
Unhealthy diet: Diets high in saturated fat, trans fat, added sugar, and sodium
push cholesterol and blood pressure in the wrong direction. -
Chronic inflammation and certain conditions: Autoimmune diseases, chronic kidney
disease, and long-term stress can all amplify vascular inflammation.
A single risk factor is concerning; multiple risk factors together dramatically raise the chance
of serious cardiovascular events. The flip side: improving even one risk factor still
helps.
Symptoms of atherosclerosis: often silent, sometimes dramatic
One of the toughest things about atherosclerosis is that it can be
completely silent for many years. You might feel fine while plaque quietly grows.
Symptoms typically appear once an artery is significantly narrowed or a clot suddenly blocks blood
flow.
Coronary artery disease (heart)
- Chest pain, pressure, or tightness (angina), especially with exercise or stress
- Pain that may spread to the arm, neck, jaw, or back
- Shortness of breath
- Unusual fatigue, nausea, or lightheadedness (especially common warning signs in women)
In a heart attack, these symptoms often become sudden, severe, and do not go away with rest. This
is a medical emergency.
Carotid and brain arteries
Reduced or blocked blood flow to the brain can cause a stroke or transient ischemic attack (TIA).
Warning signs include:
- Sudden weakness or numbness on one side of the body
- Sudden confusion, trouble speaking, or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden difficulty walking, dizziness, or loss of balance
- Sudden severe headache with no obvious cause
Call emergency services immediately if these symptoms appear, even if they go away.
Peripheral artery disease (legs and arms)
- Pain, cramping, or heaviness in the legs during walking that improves with rest (claudication)
- Cold feet or lower legs, or color changes
- Slow-healing sores or wounds on toes, feet, or legs
- Weak or absent pulses in the feet
Renal artery and aortic involvement
- Hard-to-control high blood pressure
- Worsening kidney function on blood tests
- Deep, persistent abdominal or back pain, especially if related to an aortic aneurysm
Notice a trend? Atherosclerosis often becomes obvious only when blood flow drops below what the
tissues needor when a clot suddenly shuts things down.
Potential complications
Left unchecked, atherosclerosis can lead to serious and sometimes life-threatening complications:
- Heart attack
- Stroke or transient ischemic attack (mini-stroke)
- Coronary artery disease and heart failure
- Peripheral artery disease, chronic leg pain, and non-healing ulcers
- Critical limb ischemia and risk of amputation
- Chronic kidney disease and kidney failure
- Aortic aneurysm and risk of rupture
That’s the heavy part. Now, let’s talk about how doctors find atherosclerosis and what can be done
about it.
How atherosclerosis is diagnosed
There’s no single “plaque meter” test, so healthcare professionals use a mix of history, physical
exam, and imaging or lab tests:
-
Medical history and exam: Your doctor will ask about symptoms, risk factors,
family history, and will listen to your heart and arteries for abnormal sounds. -
Blood tests: Cholesterol levels, blood sugar, kidney function, and markers of
inflammation can all give clues. -
Electrocardiogram (ECG): Records the electrical activity of your heart and can
show evidence of reduced blood flow or past heart attacks. - Stress testing: Evaluates how your heart performs under physical or medication-induced stress.
-
Ultrasound (e.g., carotid or leg arteries): Shows blood flow and can visualize
narrowing or blockages. -
Coronary calcium scoring (CT scan): Measures calcium deposits in coronary
arteries as a sign of plaque. -
CT angiography or conventional angiography: Uses contrast dye and imaging to
directly visualize narrowed or blocked arteries.
Which tests you get depends on your symptoms and overall risk profile. For many people, the first
clue is actually an abnormal cholesterol panel or high blood pressure check at a routine visit.
Treatment: slowing, stabilizing, and sometimes opening arteries
There is no magic eraser that instantly wipes plaque away, but treatment can:
- Slow or stop plaque progression
- Stabilize plaques so they’re less likely to rupture
- Improve blood flow to tissues and organs
- Reduce the risk of heart attacks, strokes, and other complications
Lifestyle changes (the foundation)
-
Heart-healthy eating: Emphasize vegetables, fruits, whole grains, beans, nuts,
lean proteins, and healthy fats (such as olive oil and fatty fish). Limit saturated fat, trans
fat, added sugars, and excess salt. -
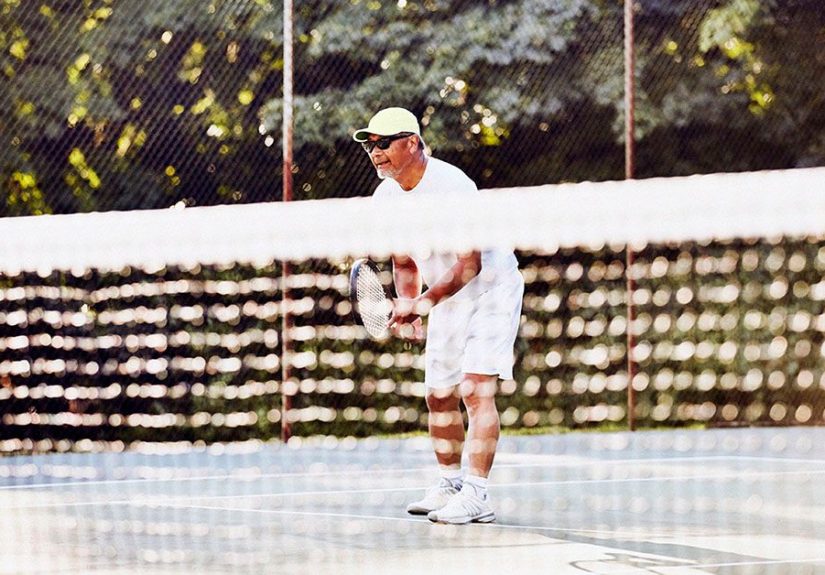
Regular physical activity: Aim for at least 150 minutes a week of moderate
exercise (like brisk walking), plus muscle-strengthening exercises on 2 or more days. Always
tailor activity to your abilities and medical advice. -
Smoking cessation: Quitting smoking (including vaping nicotine) is one of the
fastest ways to cut cardiovascular risk. Medications and counseling can make this easier. -
Weight management: Even modest weight loss can improve blood pressure, blood
sugar, and cholesterol. -
Stress and sleep: Chronic stress and poor sleep can aggravate blood pressure,
blood sugar, and inflammation. Relaxation techniques, therapy, and good sleep habits all help.
Medications
Many people with atherosclerosis or high risk of it benefit from one or more medications:
-
Statins and other cholesterol-lowering drugs: Lower LDL cholesterol and help
stabilize plaques. -
Blood pressure medications: ACE inhibitors, ARBs, calcium channel blockers, and
diuretics can protect arteries and the heart. -
Antiplatelet drugs: Aspirin or other antiplatelet agents may be used to reduce
the risk of clots forming on plaque. -
Medications for diabetes: Good blood sugar control protects blood vessels and
reduces complications. -
Other therapies: Depending on your situation, newer cholesterol drugs or
medications targeting triglycerides or inflammation may be recommended.
These medications aren’t a free pass to ignore lifestyle changesthink of them as powerful backup
singers to your healthy-habits lead vocals.
Procedures and surgeries
When arteries are severely narrowed or blocked, or when symptoms are serious, doctors may
recommend:
-
Angioplasty and stenting: A tiny balloon is inflated inside the narrowed artery
and often followed by placing a stent (a small mesh tube) to keep the artery open. -
Bypass surgery: Surgeons create a “detour” around blocked arteries using a vein
or artery from another part of your body. -
Endarterectomy: In some carotid artery disease cases, plaque is surgically
removed from the artery.
The goal of all these approaches is the same: restore and maintain enough blood flow to keep
organs and tissues happy and reduce the risk of life-threatening events.
Prevention and everyday heart-healthy habits
Whether you already have atherosclerosis or you’re trying to avoid it, the same daily habits make
a big difference:
- Get regular checkups and know your numbers: blood pressure, cholesterol, blood sugar.
- Choose mostly whole, minimally processed foods.
- Move your body throughout the day, not just during a single workout.
- Don’t smokeand if you do, seek help to quit.
- Manage stress with tools that actually help: movement, therapy, breathing exercises, social connection.
- Take prescribed medications consistently and discuss any side effects with your healthcare team.
These habits aren’t about perfection; they’re about steady, realistic improvements that your
arteries quietly appreciate over time.
Real-life experiences and practical lessons
Medical facts are important, but atherosclerosis becomes very real when you see how it plays out
in everyday life. Here are some composite, realistic examples that capture what many people
experiencenames and details changed, of course.
“I thought I was just out of shape” – the slow reveal
Mark is 54, works at a desk, and used to play pickup basketball in his 30s. Over time, work got
busier, the gym visits got rarer, and takeout became a food group. Recently, he noticed a tight,
squeezing feeling in his chest when hurrying through the airport or climbing stairs. It went away
when he stopped, so he shrugged it off as “I really need to work out more.”
At his partner’s insistence, he finally saw a doctor. His blood pressure was high, his LDL
cholesterol was elevated, and his family history included early heart disease. A stress test
suggested reduced blood flow to part of his heart. Further testing confirmed significant coronary
artery disease due to atherosclerosis.
The turning point wasn’t just the diagnosis; it was the realization that the warning signs had
been there for years: expanding waistline, creeping blood pressure, steadily rising cholesterol
numbers. Mark started medications, but he also made structured lifestyle changesdaily walks,
cooking at home most nights, and joining a smoking-cessation program. Six months later, his energy
improved, chest discomfort decreased, and his cholesterol and blood pressure were much better
controlled.
“My legs hurt, so I stopped walking” – and why that’s backwards
Linda, 67, loved going to local markets, but she’d begun to feel cramping in her calves every time
she walked more than a block or two. The pain eased with rest, so she simply started walking less
and driving more. She assumed it was “just age” or maybe arthritis.
At a routine checkup, her doctor checked pulses in her feet and ordered an ankle-brachial index
(ABI) test, which compares blood pressure in the ankle to the arm. The results showed peripheral
artery disease from atherosclerosis in her leg arteries.
The surprising prescription? A supervised walking program. By walking until the leg pain started,
resting, and then repeating the cycle under guidance, she gradually improved her circulation.
Combined with a cholesterol-lowering medication, blood pressure control, and quitting smoking, her
walking distance increased over time. Instead of avoiding activity because of pain, she learned
that the right kind of activity was part of the treatment.
“But I feel fine” – the hidden risk
Then there’s Chris, 42, who felt perfectly healthy. No chest pain, no shortness of breath. But a
workplace screening revealed significantly high LDL cholesterol and elevated blood pressure. His
father had a heart attack at 50, and his older sister recently developed diabetes.
At first, he was tempted to ignore it. After all, he could still jog and felt energetic. But after
a frank conversation with his healthcare provider, he realized that atherosclerosis often progresses silently. The goal was to act before symptoms ever appeared.
Chris agreed to start a statin, cleaned up his diet, began tracking his daily steps, and made
sleep a priority. Over the next year, his cholesterol numbers moved into a safer range, blood
pressure came down, and his long-term risk calculations looked much better. He still doesn’t “feel
sick”and that’s exactly the point. Preventive care is most powerful when nothing dramatic is
happening.
What these experiences have in common
- Atherosclerosis often builds silently until symptoms or screening reveal it.
- Symptomslike chest pain or leg crampsare easy to downplay or misinterpret.
- Family history, lab results, and blood pressure readings are crucial clues.
- Medications help, but lasting progress usually involves lifestyle changes as well.
- Small, consistent changes are more sustainable (and effective) than extreme short-term fixes.
If any of these stories feel uncomfortably familiar, take them as a nudgenot a verdict. The goal
isn’t blame; it’s awareness and action. Atherosclerosis is serious, but it’s not a one-way road.
With earlier detection and steady changes, you can significantly lower your risk and protect your
heart, brain, and limbs.
When to talk to a healthcare professional
Reach out to a healthcare professional if you:
- Have chest pain, pressure, or discomfort, especially with activity
- Notice shortness of breath, unusual fatigue, or rapid heartbeat
- Develop leg pain while walking that improves with rest
- See wounds on your feet or legs that heal slowly
- Have multiple risk factors such as high blood pressure, high cholesterol, diabetes, or a strong family history
And remember: sudden signs of heart attack or stroke are emergencies. Don’t drive yourself; call
emergency services right away.
Bottom line
Atherosclerosis is a slow-moving but powerful process that can affect arteries throughout the
body. It’s closely linked to familiar risk factorscholesterol, blood pressure, smoking, diabetes,
and inactivitybut also highly responsive to change. You may not feel plaque forming, but every
healthy meal, walk around the block, smoke-free day, and well-managed blood pressure reading is a
quiet investment in clearer, more flexible arteries.
You don’t need to become a perfect health robot. You just need to nudge your daily habits in a
heart-friendly direction and work with your healthcare team to manage your risk. Your future self
(and your arteries) will thank you.