Table of Contents >> Show >> Hide
- What are “holes in the tonsils,” exactly?
- Common causes of holes in tonsils
- 1) Normal tonsillar crypts (the “this might be totally fine” scenario)
- 2) Tonsil stones (tonsilloliths)
- 3) Tonsillitis (viral or bacterial infection)
- 4) Strep throat (group A streptococcal pharyngitis)
- 5) Infectious mononucleosis (“mono”)
- 6) Tonsillar cellulitis or peritonsillar abscess (less common, more urgent)
- 7) Ongoing irritation: postnasal drip, allergies, reflux, smoking
- Symptoms: what you might notice (and what it usually means)
- How clinicians diagnose the cause
- Treatment: what actually helps (and what to skip)
- Prevention: keeping crypts from becoming “cluttered”
- When to see a healthcare professional
- Real-life experiences: what people commonly report (and what it can teach you)
If you’ve ever looked in the mirror mid-yawn and thought, “Why do my tonsils look like tiny craters on the moon?”
you’re not alone. Those “holes” are usually tonsillar cryptsnormal little pockets in the tonsils.
Most of the time they’re harmless. The catch is that crypts can also become the perfect Airbnb for debris, bacteria,
and mucus… which is how tonsil stones (tonsilloliths) and repeated irritation can enter the chat.
This guide breaks down what holes in tonsils typically mean, what symptoms to watch for, how clinicians figure out
what’s going on, and which treatments actually help (without turning your bathroom into a DIY throat excavation site).
What are “holes in the tonsils,” exactly?
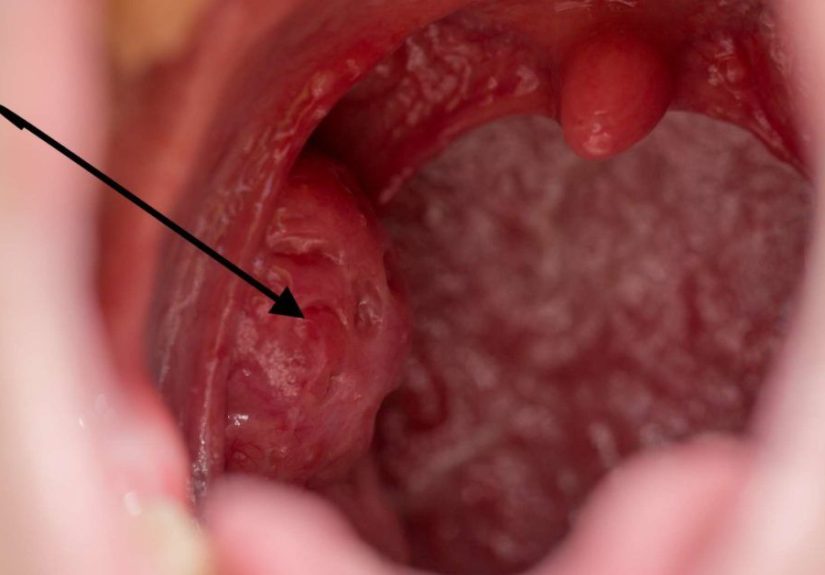
The tonsils are lymph tissue at the back of the throatpart of your immune “front desk” that samples what comes in
through your mouth and nose. Their surface isn’t smooth. It has folds and pits called crypts.
When people say “holes in my tonsils,” they’re usually describing:
- Normal crypts that are more visible than usual (some people naturally have deeper crypts).
- Enlarged crypts after inflammation or infection (swelling can make pits look more dramatic).
- Pits holding debrisoften seen as white/yellow specks or lumps (tonsil stones).
- Healing/scarring from repeated infections that changes the tonsil surface over time.
Common causes of holes in tonsils
1) Normal tonsillar crypts (the “this might be totally fine” scenario)
Many healthy tonsils have visible crypts, especially if you shine a bright light and go full detective mode.
If you feel fine and don’t have other symptoms, visible crypts alone usually aren’t a medical emergencyor even a problem.
2) Tonsil stones (tonsilloliths)
Tonsil stones form when material gets trapped in cryptsfood particles, dead cells, mucus, and bacteria
and gradually hardens (often with calcium salts). Some stones are tiny and silent. Others are bold, dramatic,
and determined to be noticed in selfies.
Risk factors can include deep crypts, a history of tonsillitis, postnasal drip, and anything that increases mouth/throat
debris or bacterial buildup.
3) Tonsillitis (viral or bacterial infection)
Tonsillitis means the tonsils are inflamed, usually because of an infection. Viral causes are common,
and bacterial causes include group A strep. When tonsils swell, crypts can look bigger or more “hole-like.”
You may also see white patches or coating (exudate), which can be confused with stones.
4) Strep throat (group A streptococcal pharyngitis)
Strep throat can cause sore throat, fever, swollen tonsils (sometimes with white patches), and tender neck lymph nodes.
The key point: you can’t reliably diagnose strep just by looking. Testing (rapid test and/or culture)
is the standard way to confirm itand antibiotics are used when it’s confirmed.
5) Infectious mononucleosis (“mono”)
Mono (often caused by Epstein-Barr virus) can cause significant throat symptoms: sore throat, fatigue, fever,
swollen lymph nodes, and tonsils that may appear enlarged and coated. This can make tonsils look lumpy, cratered,
and generally offended.
6) Tonsillar cellulitis or peritonsillar abscess (less common, more urgent)
Sometimes a bacterial infection spreads around the tonsil or forms an abscess (a pocket of pus).
This can cause severe one-sided throat pain, muffled “hot potato” voice, drooling, trouble opening the mouth,
and difficulty swallowing. If breathing feels hard or you can’t swallow fluids, that’s urgent.
7) Ongoing irritation: postnasal drip, allergies, reflux, smoking
Chronic irritation can inflame tonsil tissue and make crypts more noticeable. Postnasal drip can feed the cycle by
coating the throat with mucus; reflux can irritate the back of the throat; smoking can inflame tissues and worsen symptoms.
These don’t “drill holes,” but they can make existing crypts more obvious and more likely to trap gunk.
Symptoms: what you might notice (and what it usually means)
When it’s often benign
- Visible crypts but no pain, no fever, no swelling, no bad breath.
- Occasional tiny white speck that comes and goes with gargling or brushing.
Symptoms commonly linked to tonsil stones
- Bad breath (halitosis) or bad taste that won’t quit
- Feeling like something is stuck in your throat
- White or yellow lumps you may cough up
- Mild sore throat, cough, hoarseness, or ear discomfort (referred sensation)
Symptoms more consistent with infection (tonsillitis, strep, mono)
- Sore throat (often significant)
- Fever
- Swollen, tender lymph nodes in the neck
- Red, swollen tonsils; sometimes white/yellow coating or patches
- Trouble swallowing; fatigue (especially with mono)
Red flags: get urgent care
- Difficulty breathing, noisy breathing, or drooling
- Severe one-sided throat pain, muffled voice, or trouble opening the mouth
- Dehydration from inability to swallow fluids
- Persistent symptoms beyond about a week, or frequent recurrences
- Unexplained weight loss, a neck mass, or persistent one-sided tonsil enlargement
How clinicians diagnose the cause
Diagnosis usually starts with a history (symptoms, timeline, recurrences) and a throat exam. Depending on what’s seen
and what you report, clinicians may add:
- Rapid strep test and/or throat culture to confirm group A strep
- Mono testing and sometimes bloodwork if symptoms fit
- Assessment for complications (like an abscess) if severe symptoms are present
- Occasionally imaging if an abscess or deeper infection is suspected
A helpful rule of thumb: white stuff on tonsils is a clue, not a diagnosis. Stones, strep, and mono can
all look similar at a glance, which is why testing matters when symptoms are significant.
Treatment: what actually helps (and what to skip)
At-home care for mild symptoms or tonsil stones
- Warm saltwater gargles: can soothe irritation and help loosen small debris.
- Hydration: a drier mouth/throat can make buildup worse. Water helps.
- Oral hygiene upgrades: brush twice daily, floss, and don’t ignore the tongue.
- After-meal rinse: swishing water can reduce leftover particles that might lodge in crypts.
- Humidifier at night: helpful if dry air is irritating your throat.
About “removing” tonsil stones at home: Some people can gently dislodge small stones with coughing,
gargling, or low-pressure irrigation. If you try anything manual, keep it gentle and stop immediately if you have pain
or bleeding. Avoid sharp tools. If stones are frequent, large, painful, or hard to reach, a clinician can remove them
more safely in-office.
Treating tonsillitis
Treatment depends on the cause. Viral infections are common and usually improve with supportive care:
rest, fluids, soothing foods (warm broths or cold treats), saltwater gargles, and over-the-counter pain relievers used
as directed on the label (and with guidance from a clinician for children).
If testing confirms strep throat, clinicians typically prescribe antibiotics (commonly penicillin-class
medications). This helps reduce complications and can shorten illness and contagiousness when started promptly.
Don’t use leftover antibiotics or share prescriptionswrong meds and wrong duration can cause real problems.
Treating mono
Mono is usually managed with supportive care: rest, hydration, and symptom relief. Fatigue can be intense and may linger.
Because mono can enlarge the spleen in some people, clinicians often advise avoiding contact sports until cleared.
If throat swelling is severe, a clinician may consider additional treatments based on your situation.
When an abscess is suspected
A peritonsillar abscess (or severe cellulitis) needs prompt medical evaluation. Treatment may include drainage and
antibiotics, and clinicians focus on protecting the airway and restoring hydration.
What if this keeps happening? (recurrent tonsillitis and ENT options)
If you’re getting repeated significant infections, an ENT may discuss whether tonsil removal (tonsillectomy) makes sense.
Decision-making often considers how many documented episodes you’ve had, how severe they were, and how much they disrupt life.
In children, commonly referenced criteria include thresholds like multiple episodes per year over multiple years,
with documentation of key features (fever, swollen nodes, tonsillar exudate, positive strep test).
For frequent, bothersome tonsil stones, clinicians may recommend prevention strategies first. In stubborn cases,
procedural options can be discussed, including tonsillectomy when symptoms are persistent and significantly affect quality of life.
Prevention: keeping crypts from becoming “cluttered”
- Brush and floss consistently (bacteria love chaos).
- Hydrate and manage dry mouth.
- Address postnasal drip with clinician-approved allergy strategies if it’s chronic.
- Manage reflux if you have frequent heartburn, throat clearing, or morning hoarseness.
- Avoid smoking/vapingit irritates tissues and can worsen throat symptoms.
- Regular dental care helps reduce bacterial load that contributes to bad breath and buildup.
When to see a healthcare professional
Consider getting checked if you have:
- Fever, severe sore throat, or swollen neck glands
- Symptoms lasting longer than about a week or worsening rapidly
- Repeated “tonsil episodes” that disrupt school, work, or sleep
- Large, painful, or frequently recurring tonsil stones
- Any red-flag symptoms like trouble breathing, drooling, or severe one-sided throat pain
Real-life experiences: what people commonly report (and what it can teach you)
People rarely describe “holes in my tonsils” the same way twicebecause the experience is often less about the holes
and more about what’s happening in them. One common story goes like this: someone notices a stubborn bad taste
and breath that no amount of brushing seems to fix. They drink water, chew gum, and panic-text a friend,
then finally shine a phone flashlight into their mouth and spot a tiny white dot. The dot turns out to be a small
tonsil stoneannoying, but not dangerous. The relief is immediate: not because the problem is glamorous,
but because it’s explainable.
Another frequent experience is the “post-illness surprise.” After a bout of tonsillitis or a nasty sore throat,
the tonsils can look different: more pitted, more textured, and easier to scrutinize. Some people interpret this as
“damage” or a permanent new problem. In reality, inflammation can make crypts look deeper for a while, and healing
can change the surface slightly. If symptoms fade and you’re otherwise well, the mirror can be more alarming than the anatomy.
(The mirror is not always your friend. Sometimes it’s just a drama coach.)
People with allergies often describe a pattern: mornings are worse, throat clearing is constant, and crypts seem to
“collect” more stuff. They’ll say the holes feel more noticeable when postnasal drip is activealmost like the tonsils
are doing extra chores. When they get allergy symptoms under control, the tonsils often feel calmer too. It’s not that
allergies create holes; it’s that mucus and irritation make normal crypts more likely to trap debris.
Then there’s the “I thought it was a stone, but it was an infection” experience. Some people see white patches and assume
tonsil stonesuntil the fever, body aches, and intense pain show up. That’s when testing matters. Strep throat and mono
can look similar visually, and both can cause dramatic tonsil changes. People who’ve been through it often say the turning
point was seeking care when symptoms were more than mild annoyance: high fever, significant swelling, trouble swallowing,
or fatigue that felt out of proportion.
Finally, for people with frequent recurrencesmultiple bad throat infections a yearthe experience is often about
quality of life. They describe missed school/work, disrupted sleep, and a sense of dread whenever a sore throat starts.
When they talk with an ENT, the conversation becomes less about “holes” and more about the pattern: frequency, severity,
documentation, and whether the tonsils are causing more trouble than they prevent. Some end up managing well with prevention
and targeted care; others choose tonsillectomy after careful evaluation. The most consistent takeaway from these stories is
simple: the best plan is the one that matches your symptoms, not just what you see in the mirror.






