Table of Contents >> Show >> Hide
- At-a-glance comparison
- X-rays: the original quick look
- CT scans: speed plus high-resolution anatomy
- MRI: soft-tissue superstar (no ionizing radiation)
- Ultrasound: sound waves and live views
- Nuclear medicine: PET and SPECT (functional imaging)
- Mammography (2D & 3D tomosynthesis)
- DEXA (bone density): quick, very low dose
- Fluoroscopy and interventional imaging: motion pictures for medicine
- How doctors choose the right scan (common scenarios)
- Contrast agents: the “highlighters” of imaging
- Preparing for your scan
- After the scan: what to expect
- Understanding your radiology report
- FAQs (fast, friendly answers)
- Bottom line
- SEO wrap-up
- of real-world experience & tips
Medical imaging is like the smartphone camera of modern medicinesame idea (snap a pic), wildly different tech under the hood. From X-rays and CT to MRI, ultrasound, and nuclear medicine (PET/SPECT), each scan answers a specific question. This guide breaks down what each test does best, when doctors commonly use it, what it feels like, and how to prepso you can walk into your scan confident, not confused.
At-a-glance comparison
| Modality | Best for | Typical uses | Ionizing radiation? | Contrast sometimes used? | Speed |
|---|---|---|---|---|---|
| X-ray | Bone, lungs, quick checks | Fractures, pneumonia, dental films | Yes (low) | Rarely | Minutes |
| CT (Computed Tomography) | Detailed anatomy, emergencies | Trauma, stroke, chest/abdomen, kidney stones | Yes | Often (iodine-based) | Minutes |
| MRI (Magnetic Resonance Imaging) | Soft tissue detail | Brain/spine, joints, ligaments, liver, pelvis | No | Sometimes (gadolinium-based) | 30–60+ minutes |
| Ultrasound | Soft tissues, blood flow | Pregnancy, gallbladder, thyroid, vessels | No | No (gel only) | Minutes |
| PET/SPECT (Nuclear Medicine) | Function/metabolism | Cancer staging, heart perfusion, thyroid, bone scan | Yes (from radiotracer) | Radiotracer is the “contrast” | Hours (includes uptake time) |
| Mammography (2D/3D) | Breast screening & diagnosis | Routine screening, workup of breast symptoms | Yes (very low) | No (occasionally with contrast for special studies) | Minutes |
| DEXA (Bone Density) | Bone mineral density | Osteoporosis screening & monitoring | Yes (very low) | No | Minutes |
| Fluoroscopy | Real-time X-ray | GI studies, joint injections, procedures | Yes | Often | Varies |
X-rays: the original quick look
What it is: A fast shot of your insides using a tiny burst of ionizing radiation. Think skeleton selfies and lung postcards.
Great for: Bones (fractures, arthritis), lungs (pneumonia, fluid), and quick checks after an injury.
Radiation: Very low; a typical chest X-ray is commonly cited around about a tenth of a millisievertroughly the same ballpark as several days of natural background radiation. Your provider orders X-rays when benefits outweigh that small exposure.
What it’s like: You stand or lie still for a few seconds. No special prep, no recovery time, and you can drive home.
CT scans: speed plus high-resolution anatomy
What it is: A rotating X-ray machine and powerful computer build cross-sectional “slices” of your bodyexcellent for detail in the chest, abdomen, pelvis, and head.
Great for: Emergency evaluation (head injury, stroke alerts, chest or belly pain), lung nodules, kidney stones, appendicitis, and vascular imaging with CT angiography (CTA).
Radiation: Higher than an X-ray because CT takes many images. Dose depends on the body part and protocol; scanners use dose-reduction techniques and reference levels to keep exposure as low as reasonably achievable.
Contrast: Many CTs use iodine-based contrast through an IV to highlight organs and blood vessels. Most people do fine; rare reactions can occur. If you’ve had a prior reaction, asthma, or severe allergies, tell the team. If you take metformin or have reduced kidney function, the staff will follow safety protocols.
Pregnancy: If the area scanned is not the abdomen or pelvis, risks to the fetus are minimal; when the belly must be imaged, your team will consider alternatives like ultrasound or MRI when appropriate.
What it’s like: You lie on a table that slides through a circular scanner. You may feel a warm flush or metallic taste if IV contrast is used. Hydrating after the exam is commonly advised unless your clinician says otherwise.
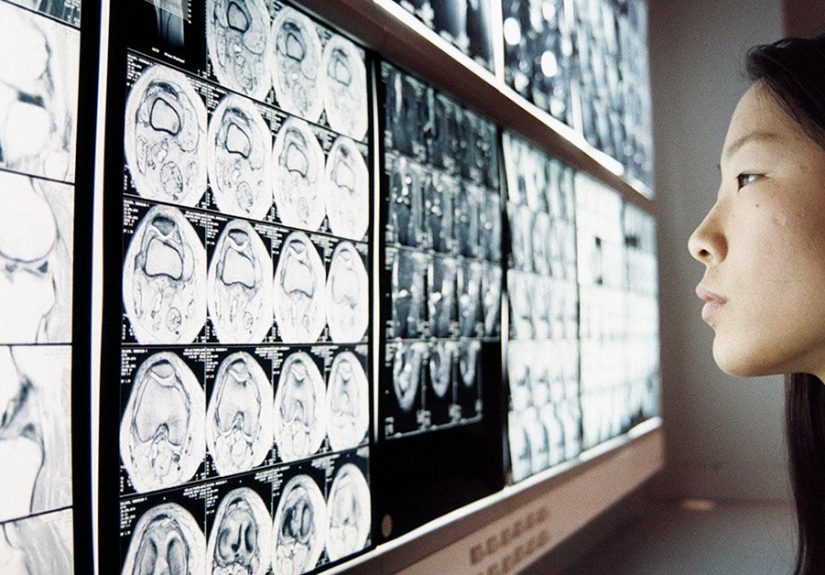
MRI: soft-tissue superstar (no ionizing radiation)
What it is: A strong magnet, radio waves, and a lot of math create detailed pictures of soft tissuesbrain, nerves, joints, pelvic organs, liver, and morewithout ionizing radiation.
Great for: Subtle brain findings, spinal discs and nerves, ligament and tendon injuries, pelvic and liver lesions, and MR angiography for vessels.
Safety: MRI is safe for most people, but the magnet can interact with some metal implants and devices. Always tell the team about stents, pacemakers, cochlear implants, clips, or shrapnel. Many implants are now labeled MR Safe or MR Conditional; MR-Unsafe devices generally mean no MRI.
Contrast: MRI sometimes uses gadolinium-based contrast. For most patients, it’s well tolerated; if your kidney function is severely reduced, the team selects the safest agent or avoids it. Tiny traces of gadolinium can be retained in tissues; no harmful effects have been demonstrated at typical clinical doses with modern agents, but radiologists factor this into decisions.
What it’s like: Expect a narrow tube, loud rhythmic knocking, and staying still. Claustrophobic? Ask about music, a mirror periscope, mild sedation, or “open” MRI options when available.
Ultrasound: sound waves and live views
What it is: A handheld probe sends sound waves and “listens” for echoes to form imagesno radiation, widely available, and great for real-time imaging.
Great for: Pregnancy, gallbladder, kidneys, thyroid, soft-tissue lumps, and vascular flow with Doppler. In kids and in pregnancy, ultrasound often comes first because it’s safe and quick.
Limitations: Image quality can vary by body habitus and operator skill; air and bone block sound, so lungs and certain deep structures can be tricky.
What it’s like: Clear gel + gentle pressure. Usually no prep, and you can resume normal activity immediately.
Nuclear medicine: PET and SPECT (functional imaging)
What it is: You receive a small amount of a radioactive tracer that targets specific tissues. Special cameras detect where it goes to reveal physiology (metabolism, perfusion), not just anatomy.
Great for: Cancer staging and treatment response (FDG-PET), cardiac perfusion, bone scans, thyroid evaluation, and detecting infection/inflammation in certain cases.
Radiation: Yes, from the tracer. The radioactivity fades naturally and often passes in urine/stool; drinking water afterward is commonly advised unless you have fluid restrictions.
What it’s like: After tracer injection, there’s a quiet “uptake” period before imaging. The scan itself is painless; you’ll be asked to lie still.
Mammography (2D & 3D tomosynthesis)
What it is: Low-dose X-ray of the breast. 3D mammography (tomosynthesis) acquires many thin “slices,” helping radiologists see through overlapping tissue.
Screening guidance (average risk): Many organizations now recommend starting routine screening at age 40, typically every other year through 74 for average-risk women. Some clinics still advise annual screening; talk with your clinician about your personal risk profile.
What it’s like: Brief compression (deep breath helps!). If you have dense breasts, 3D may reduce call-backs; supplemental ultrasound or MRI may be considered based on risk and local practice.
DEXA (bone density): quick, very low dose
What it is: A dual-energy X-ray that measures bone mineral density in the spine and hips. You’ll see T-scores and Z-scores in your report; T-scores help diagnose osteoporosis and guide treatment.
Great for: Screening and monitoring osteoporosis risk, especially after menopause, with certain medications, or with fracture history.
What it’s like: You lie still for a few minutes. No injections, no IV, no special prep.
Fluoroscopy and interventional imaging: motion pictures for medicine
What it is: Real-time X-ray used for GI studies (like barium swallow), joint injections, or image-guided procedures. Because fluoroscopy can run longer than a single X-ray, teams minimize exposure with time, distance, and shielding.
What it’s like: You may swallow contrast for GI exams or get local anesthesia for procedures. Afterward, you’ll receive simple care instructions.
How doctors choose the right scan (common scenarios)
- Head injury or stroke alert: CT is fast and great for bleeding; MRI may follow for finer detail.
- Joint or ligament injury: MRI shows soft tissues best; X-ray may still check for fractures.
- Kidney stones: Non-contrast CT is often used; ultrasound may be used first in pregnancy.
- Appendicitis: Ultrasound often first in kids and pregnancy; CT is common in adults.
- Breast screening: Mammography (2D or 3D) at routine intervals; MRI may be added for high-risk patients.
- Cancer staging: CT for anatomy; PET/CT to assess metabolic activity and treatment response.
Important: These are typical patterns, not personal medical advice. Your clinician tailors imaging to your symptoms, history, and risks.
Contrast agents: the “highlighters” of imaging
Iodinated contrast (CT/X-ray)
Helps show blood vessels and organs. Reactions are uncommon; most are mild and treatable. If you had a prior reaction, tell the teampremedication or an alternative may be considered. If kidney function is reduced, teams adjust decisions and hydration plans. In infants and very young children, special thyroid monitoring guidance exists when iodinated contrast is used.
Gadolinium contrast (MRI)
Modern (Group II) gadolinium agents have a very low risk of nephrogenic systemic fibrosis in advanced kidney disease; your team selects agents accordingly. Trace tissue retention has been observed, but no harmful effects have been shown at routine diagnostic doses with contemporary agents. As always, risk-benefit is individualized.
Preparing for your scan
- Clothing & metal: Wear comfy, metal-free clothing; remove jewelry for CT/MRI.
- Implants & devices: Bring your implant card (pacemaker, cochlear implant, aneurysm clip, insulin pump, etc.). This is crucial for MRI safety.
- Food & drink: Some CTs require fasting; others don’t. Follow your prep sheet. If you receive contrast and have no fluid restriction, drinking water after the exam is commonly advised.
- Medications: Keep taking your meds unless told otherwise. Metformin users may follow special instructions based on kidney function.
- Pregnancy & breastfeeding: Tell the technologist if you may be pregnant or are breastfeeding; plans will be adjusted if needed.
- Claustrophobia: Ask about comfort options for MRI (music, mirror, mild sedation, or open MRI where available).
After the scan: what to expect
Most scans let you resume normal activity right away. For PET/SPECT, you might be asked to limit close contact with pregnant people or infants for a short period and to stay well hydrated unless advised otherwise. If contrast was used and you notice rash, trouble breathing, persistent pain at the IV site, or anything worrying, contact your care team.
Understanding your radiology report
Your report summarizes technique, findings, and impressions. “Impression” is the bottom line; it lists the most important results and recommendations. It’s written for doctors, so don’t hesitate to ask your clinician to translate.
FAQs (fast, friendly answers)
Will a CT or X-ray give me too much radiation? Medical teams weigh benefits vs. the small risks and use the lowest dose for quality images. Sometimes imaging prevents bigger risks by speeding diagnosis.
Can I get an MRI with metal in my body? Often yesif your device is MR Safe or MR Conditional and protocols are followed. If it’s MR-Unsafe or unknown, your team will pick another test or verify details first.
Is ultrasound always safer? It uses no ionizing radiation and is generally considered safe when used appropriately by trained professionals. It’s fantastic for many questions, but not every question.
Bottom line
No single scan is “best” for everything. Each modality has strengths, trade-offs, and safety considerations. With the right test for the right question, imaging can speed diagnosis, steer treatment, and spare you unnecessary procedures.
SEO wrap-up
sapo: Confused about medical imaging? This friendly deep-dive compares X-rays, CT, MRI, ultrasound, nuclear medicine, mammograms, and DEXA. Learn what each scan shows best, how to prepare, common safety questions, and how doctors choose the right testso you feel informed before you step into the scanner.
of real-world experience & tips
From the waiting room to the “all done,” here’s what patients and technologists often say makes imaging smoother. First, timing and prep matter more than you think. If your CT requires fasting or oral contrast, build in a little extra time. Oral contrast tastes better than it used to (low bar, we know), but chilling it and sipping steadily helps. If your scan involves IV contrast, warming blankets and deep, relaxed breathing can minimize that brief “whoosh of warmth.” Hydrationwhen not fluid-restrictedhelps you feel better afterward and supports your kidneys as they clear the contrast.
For MRI newbies: the sounds are normalthink techno drumline meets construction site. Ask for ear protection plus music; a good playlist makes the time pass faster. If you’re claustrophobic, request a mirror periscope so you can see out of the bore, and try a “practice breath” session to get used to staying still. Focus on slow, paced breathing (count to four in, six out); it reduces fidgeting and motion blur, which means fewer repeats. If your facility offers it, an “open” or wider-bore MRI can feel dramatically easier, though image quality and availability vary.
Bringing an implant card pays off. Pacemaker? Cochlear implant? Aneurysm clip? Insulin pump? Show the card to registration and the technologistthis can save time verifying device make/model and ensure the correct safety protocol. Even some wearables and continuous glucose monitors have specific imaging guidance; letting the team know upfront helps them decide whether devices can stay on or need temporary removal.
Ultrasound hacks: Wear a two-piece outfit if you’re having an abdominal or pelvic ultrasound; it’s easier to expose just what’s needed. If you’re scheduled for a vascular ultrasound of the legs, don’t apply lotions the day of the examslippery skin can make probe contact harder and lengthen the test.
For PET/SPECT: The “uptake” time is your frienduse it to relax. Follow diet/activity instructions closely (for FDG-PET, that often means keeping muscles quiet so they don’t “hog” the tracer). After the scan, common advice is to hydrate unless you’ve been told to restrict fluids; short-term distancing from pregnant loved ones or infants may be recommendedask your technologist.
Mammogram confidence builders: Schedule when breasts are least tender (often the week after your period). Skip deodorant and powders on exam day to avoid artifacts. If you’re nervous about discomfort, ask the technologist to coach your breathinggentle, even breaths can help muscles relax and ease compression.
Read your prep sheet like a pro: Many “bad scan days” start with missed instructions. If anything is unclearfasting rules, metformin guidance, what to wearcall the imaging center ahead of time. Write down your meds and allergies; bring the list. Finally, remember that radiology teams do this all day, every day. They’re there to keep you safe, comfortable, and get the clearest answers possible. Asking questions is not just allowedit’s smart.