Table of Contents >> Show >> Hide
- What lymphedema is (and why it happens after breast cancer treatment)
- How common is lymphedema after breast cancer surgery?
- Risk factors: who’s more likely to develop it?
- Early signs and symptoms (your “don’t ignore this” checklist)
- Why early detection matters (and what screening can look like)
- Prevention and risk reduction: what actually helps?
- Treatment options: what works for lymphedema after breast cancer surgery?
- When to contact your care team urgently
- Living well with lymphedema: work, travel, exercise, and the mental load
- Bottom line
- Real-world experiences (what people commonly report, and what tends to help)
Breast cancer surgery can be life-saving. Unfortunately, it can also leave you with an uninvited “souvenir”:
lymphedema after breast cancer surgery. If you’ve noticed one sleeve suddenly feeling like it
shrank in the wash (but only on one arm), or your watch is getting suspiciously snug, you’re not aloneand
you’re not imagining it.
The good news: breast cancer–related lymphedema (often called BCRL) is manageable, especially
when it’s caught early. The even-better news: you do not have to become a full-time arm detective to handle it.
You just need a clear plan, a few smart habits, and a care team that takes swelling seriously.
What lymphedema is (and why it happens after breast cancer treatment)
Lymphedema is swelling caused by a buildup of protein-rich lymph fluid in the tissues when the lymphatic system
can’t drain efficiently. Think of your lymphatic system as your body’s “cleanup and drainage” network. When lymph
nodes or lymph vessels are removed, scarred, or damaged, fluid can pool instead of flowing back toward the trunk.
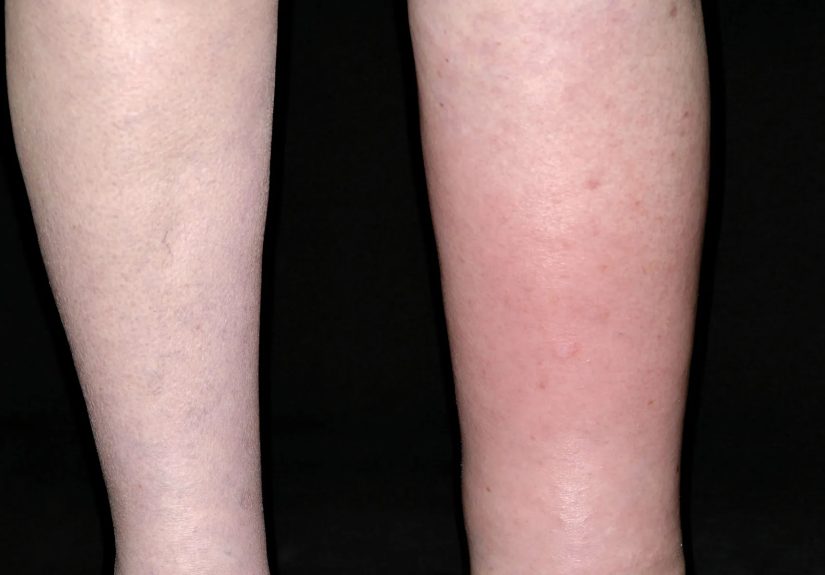
After breast cancer surgery, lymphedema most commonly shows up on the same side as treatmentoften in the
arm or hand, but it can also affect the breast, chest wall, armpit, back, or torso.
Surgery that removes lymph nodes (especially underarm/axillary nodes) and radiation that affects lymph drainage are
common triggers.
Sentinel lymph node biopsy vs. axillary lymph node dissection
Not all lymph node surgery carries the same risk. A sentinel lymph node biopsy removes fewer nodes
(the “first” nodes that would likely catch cancer cells). An axillary lymph node dissection removes
more nodes. In general, removing more nodes increases the odds that drainage pathways get disrupted, which raises the
risk of lymphedema.
How common is lymphedema after breast cancer surgery?
This is one of those questions where the honest answer is: it depends. Rates vary based on the type of
surgery, how many lymph nodes were removed, whether radiation included lymph node regions, your body weight, and
whether infections or inflammation occur in the affected area.
Many patient-focused survivorship resources report that lymphedema is less common after sentinel node biopsy and more
common after axillary dissection. Some estimates place lymphedema risk around
under 5% after sentinel node biopsy and roughly 10%–20% after axillary dissection
at about one year, though higher ranges appear in some groups and longer follow-up. The takeaway is not to memorize
a percentageit’s to know your personal risk profile and monitor early.
When does it show up?
Lymphedema often develops within the first few years after surgery, but it can also appear much latersometimes a
decade or more after treatment. That’s why survivorship follow-up isn’t just a formality; it’s part of prevention.
Risk factors: who’s more likely to develop it?
You can do everything “right” and still develop lymphedemaso please don’t turn this into a personal blame project.
That said, knowing risk factors helps you and your clinicians choose smarter prevention and screening.
Treatment-related risk factors
- More extensive lymph node removal (especially axillary lymph node dissection).
- Radiation that includes the underarm/axillary or nearby nodal regions.
- Scar tissue and reduced mobility after surgery that can affect drainage and movement patterns.
- Complications like seromas (fluid collections) or infections that increase inflammation.
Body and lifestyle-related factors
- Higher body weight (overweight/obesity is consistently associated with higher risk).
- Injury or infection in the at-risk arm/hand (even small cuts can matter if they lead to infection).
- Reduced activity and stiffness (deconditioning can make everything harderincluding lymph flow).
Early signs and symptoms (your “don’t ignore this” checklist)
Lymphedema can start subtly. Some people notice an odd sensation before visible swelling. Others see changes in fit
firstrings, sleeves, bras, or watchbands suddenly feel tighter. Early symptoms can fluctuate, which is both common
and maddening (because you’ll wonder if you made it up). You didn’t.
Common early clues
- Swelling in the arm, hand, breast, chest, or trunk on the treated side
- Heaviness, tightness, fullness, or a “puffy” feeling
- Skin tightness or changes in texture
- Aching, discomfort, or reduced range of motion
- Clothing or jewelry fitting differently on one side
If you’re thinking, “Okay, but my arm also feels weird sometimes because bodies are weird,” fair. The practical rule
is this: new, persistent, or increasing one-sided swelling deserves a quick message or call to your
care teamespecially if you had lymph node surgery or nodal radiation.
Why early detection matters (and what screening can look like)
Lymphedema is easier to manage in earlier stages. Many centers encourage baseline measurements before or around the
time of surgery, then periodic follow-up so small changes can be caught earlybefore swelling becomes more stubborn.
How clinicians monitor for lymphedema
- Arm measurements (tape measurements at set points)
- Symptom checks during follow-up visits (tightness, heaviness, fit changes)
- Bioimpedance spectroscopy in some programs (a noninvasive way to detect fluid changes)
- Imaging in specific situations (to evaluate lymphatic flow or rule out other causes)
If your clinic doesn’t offer formal screening, you can still advocate for documentation of baseline arm size and
consistent follow-up. The goal is not perfection; it’s a reliable “before vs. after” comparison.
Prevention and risk reduction: what actually helps?
Prevention isn’t a magic spell. It’s a set of habits that reduce inflammation, lower infection risk, and keep your
arm and shoulder moving well. These steps are especially important if you had multiple nodes removed or nodal
radiation.
1) Protect your skin (because infection is a big deal)
Your skin is the front door. If bacteria get in through a cut or bite, the immune system rushes in, fluid increases,
and the lymphatic system has to handle more traffic with fewer lanes open.
- Moisturize to prevent cracking and keep skin healthy.
- Use gloves for gardening, cleaning, or anything sharp/abrasive.
- Treat cuts promptly: clean, protect, and watch for signs of infection.
- Be cautious with burns and sunburnyes, the sun can be rude to your lymphatic system.
2) Keep your shoulder and arm moving (gently, then progressively)
Movement helps lymph fluid circulate. After surgery, you’ll typically start with gentle range-of-motion exercises
guided by your surgical team or physical therapist. Over time, many survivors safely return to strength training
with a gradual, supervised approach.
In fact, research reviews and survivorship guidance increasingly support progressive resistance training as safe for
people at risk for lymphedema when it’s introduced carefully and monitored. The key phrase is
progressive and supervisednot “go from zero to overhead press because you felt brave.”
3) Compression: the “right tool at the right time”
Compression sleeves and garments can help prevent fluid from pooling and can be part of treatment. But fit matters.
A too-tight sleeve can cause problems, and an off-the-shelf guess can be hit-or-miss. If compression is recommended,
get measured by someone trained in lymphedema garment fitting.
4) Weight management (without diet-culture nonsense)
Higher body weight is associated with higher lymphedema risk and can make swelling harder to control. This is not a
moral issue; it’s biology and fluid dynamics. If weight change is part of your care plan, aim for sustainable,
health-focused support (often a mix of movement, nutrition coaching, and realistic goals).
5) What about blood draws, IVs, and blood pressure cuffs?
You’ll hear a lot of “never let anyone touch that arm again” advice. Real-world practice varies, and evidence is
nuanced. Many clinicians still recommend using the other arm when possibleespecially if you already have swelling
or you’re at higher riskbecause avoiding unnecessary trauma and infection risk is sensible.
If both arms are at risk, or there’s no alternative, don’t panic. Tell the clinician about your history and ask for
the safest option (for example, using a different site when feasible and keeping skin clean afterward).
Treatment options: what works for lymphedema after breast cancer surgery?
There’s currently no universal “one-and-done” cure, but there are highly effective ways to reduce swelling, improve
comfort, and prevent progression. The best plan depends on your stage, symptoms, and goals (work, exercise, travel,
comfort, and confidence all count as goals).
Complete decongestive therapy (CDT): the gold-standard foundation
Many cancer centers describe complete decongestive therapy (CDT) as the core approach. It usually
includes:
- Manual lymphatic drainage (MLD): a gentle, specialized technique performed by trained therapists.
- Compression: bandaging early on and/or fitted garments to maintain gains.
- Exercise: targeted movement that supports drainage and restores function.
- Skin and nail care: to reduce infection risk and protect fragile tissues.
CDT is often taught with a strong self-management componentbecause real life happens between appointments. A good
lymphedema therapist doesn’t just treat you; they teach you how to keep results going at home.
Pneumatic compression pumps
Some people benefit from a pneumatic compression devicea sleeve connected to a pump that inflates and deflates in
cycles. These devices can support fluid movement, particularly when used as part of a broader plan (not as a solo
act).
Medications
Meds don’t “drain” lymphedema. But antibiotics may be needed if there’s an infection, and pain management may be part
of symptom control. If swelling appears suddenly, your clinician may also evaluate for other causes that require
different treatment.
Surgical options (for selected cases)
When conservative therapy isn’t enough, specialized centers may consider surgeryespecially for persistent or
advanced cases. Options can include:
-
Lymphatic bypass / lymphovenous anastomosis: creating new pathways so lymph can drain into nearby
veins. -
Vascularized lymph node transfer: transplanting healthy lymph nodes to help restore drainage in the
affected region. -
Liposuction for advanced lymphedema: used in specific cases where tissue changes are prominent,
paired with ongoing compression afterward.
Surgery isn’t right for everyone, and it still usually requires ongoing management. But for some people, it can
reduce swelling and improve daily function significantlyespecially when paired with expert therapy.
When to contact your care team urgently
Call your clinician promptly if you notice rapid swelling, or if swelling comes with
redness, warmth, fever, or spreading tendernessthese can be signs of infection that needs quick
treatment. Also contact your team if you have new or worsening swelling that doesn’t improve, or if something feels
“off” compared to your usual pattern.
Living well with lymphedema: work, travel, exercise, and the mental load
Lymphedema isn’t just a physical changeit’s a planning change. People describe the mental load of remembering a
sleeve, monitoring for flare-ups, and wondering whether a long flight or a hot day will cause swelling. That’s real,
and it deserves support.
Practical day-to-day strategies
- Build a “flare-up plan”: who you call, what you do first, and what helps you calm swelling.
- Choose strength over fear: progressive exercise, guided by pros, often improves confidence and function.
- Plan for heat: hot weather can worsen swelling for some peoplethink hydration, breaks, and breathable clothing.
- Make compression realistic: comfort and fit are everything; re-check sizing over time.
If you’re struggling emotionally, you’re not being dramatic. You’re adjusting to a chronic condition after a major
life event. Support groups, survivorship clinics, and counseling can be as useful as any sleeve.
Bottom line
Lymphedema after breast cancer surgery is common enough that every survivor deserves clear education and a monitoring
plan. It can be mild or more disruptive, early or late, and it can change over time. The best outcomes usually come
from early detection, consistent self-care, and access to trained lymphedema therapyplus a realistic, sustainable
approach to movement and health.
If you suspect lymphedema, bring it up promptly. You’re not “bothering” your care teamyou’re protecting your
long-term function. And that’s the whole point of survivorship.
Real-world experiences (what people commonly report, and what tends to help)
The lived experience of breast cancer–related lymphedema is often less like a dramatic movie scene and more like a
series of tiny plot twists: a sleeve that feels tight on a humid day, a hand that looks puffy after carrying grocery
bags, or a “why does my ring hate me now?” moment that won’t quit. Many survivors say the hardest part early on is
uncertaintybecause swelling can come and go, and the line between “normal post-surgery weirdness” and “this needs
attention” isn’t always obvious.
A common theme is that the first clue is fit, not pain: a watchband gets snug, a shirt sleeve feels
tighter on one side, or a bra band rubs differently. Others describe a heaviness or fullness that’s more annoying
than painfullike your arm is wearing a slightly-too-warm sweater that you can’t take off. Some people report
frustration when swelling is mild but persistent: it doesn’t look “serious,” yet it impacts comfort, confidence, and
everyday tasks like typing, cooking, or exercise.
Many survivors also describe a learning curve with compression. The first sleeve might feel awkward,
too hot, or not quite rightespecially if it wasn’t professionally fitted. Once someone finds a garment that fits
well and matches their lifestyle (work, workouts, travel), the tone often shifts from “I hate this thing” to “Okay,
this is my seatbelt.” Not glamorous, but useful. People frequently say that a skilled lymphedema therapist is the
difference between random trial-and-error and an actual planespecially when therapy includes coaching for home care,
not just in-clinic treatment.
Exercise experiences have evolved, too. Plenty of survivors admit they were initially afraid to lift anything heavier
than a coffee mug, worried it would “trigger” swelling. Over timeoften with guidancemany find that gradual,
progressive strengthening actually improves how their arm feels and functions. It’s not about becoming a powerlifter;
it’s about getting your confidence back so normal life doesn’t feel like a risk assessment.
Some experiences highlight how specialized care matters. For example, one breast cancer survivor’s story shared by a
major cancer center described needing intensive wrapping, custom garments, and pump use after extensive lymph node
removal, followed by improvement significant enough to qualify for a lymphatic bypass procedure. Stories like this
often underline two points survivors repeat: early referral helps, and expert resources vary
by location, so it’s worth asking for a specialist when your symptoms aren’t improving.
What survivors often say they wish they’d known sooner
- “Mild” lymphedema still counts. Catching subtle changes early can prevent bigger problems later.
- You deserve a baseline. Measurements (or other screening methods) make changes easier to spot.
- Compression is a tool, not a punishment. The right fit can make it far more tolerable.
- Strength isn’t the enemy. Gradual, guided exercise often supports function and confidence.
- The mental load is real. Support groups and survivorship clinics can be as helpful as any device.
If you’re dealing with lymphedema after breast cancer surgery, the most encouraging “experience-based” takeaway is
this: many people find a rhythm. It may take a few adjustmentstherapy, garments, exercise pacing, skin care habits
but lymphedema management often becomes a routine rather than a constant emergency. And you don’t have to figure it
out alone.






